GLP-1s, Medicare, and the Wellness Industry's Grift
Why rejecting GLP-1 access isn’t about public health. It’s about protecting wellness profits
Hi - this newsletter is free to read, but a paid subscription helps to support my work. If you find it helpful, please consider upgrading to become a paid subscriber. Thanks for being here.
Over the past year, GLP-1 receptor agonists, like Ozempic, Wegovy, and Mounjaro, have sparked a cultural, medical, and economic conversation. Originally approved to help manage blood sugar in people with type 2 diabetes, these medications have demonstrated far-reaching benefits. Beyond lowering HbA1c levels, they have consistently been shown to reduce body weight, lower blood pressure, improve cholesterol levels, and reduce the risk of major cardiovascular events. For many people with obesity and related conditions, GLP-1s are not just about weight loss. They're about unlocking a path to better metabolic health, improved quality of life, and the possibility of finally gaining traction with long-recommended behavior changes like dietary shifts and regular movement.
In November 2024, the Biden administration proposed a rule to expand Medicare and Medicaid coverage of GLP-1s, citing major scientific advancements and the urgent public health need to address obesity as a chronic disease. The administration emphasized that these medications, which are shown to reduce the risk of cardiovascular events by up to 20%, could significantly improve outcomes for the more than 40% of Americans living with obesity. The proposal also pointed to the high out-of-pocket costs of GLP-1s, which can reach $1,000 per month without insurance coverage, and made the case that expanded access could reduce long-term healthcare costs by preventing diabetes, heart disease, and other complications.
But last week, the Trump administration rejected the Biden proposal, citing concerns over cost and longstanding Medicare rules prohibiting coverage for weight-loss drugs. Though GLP-1s are already covered for diabetes and certain obesity-related conditions, the proposal would have extended access to millions more. The Congressional Budget Office projected a $35 billion federal cost over 10 years, which the administration deemed "not appropriate at this time." The decision, however, runs counter to the Trump administration's own stated goal of "ending the chronic disease epidemic." GLP-1s are among the most effective tools we've seen for improving markers of conditions like hypertension, high cholesterol, and type 2 diabetes. Rejecting coverage undermines that public health commitment and forfeits a clear opportunity to improve outcomes and reduce long-term costs.
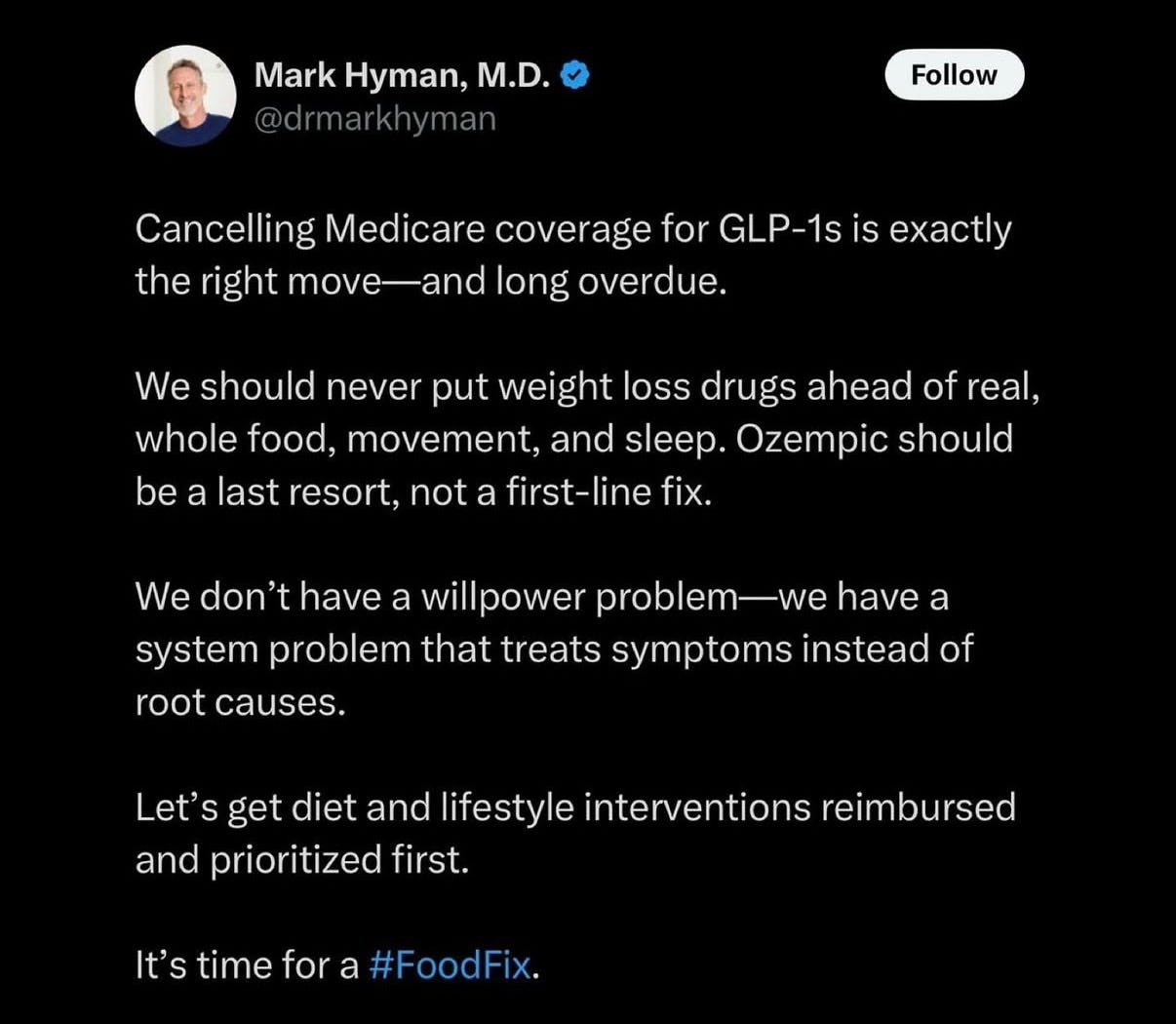
This policy reversal was quickly seized upon by MAHA supporters and figures in the wellness world, including Dr. Mark Hyman, who posted:
The Hypocrisy at the Heart of Wellness
Dr. Hyman's post is a case study in how the wellness industry creates false binaries, rewrites policy history, and critiques pharmaceutical profit while conveniently distracting from its own.
To see how this dynamic plays out, let’s break down the post, and the deeper contradictions it reveals.
1. “Long overdue” is misleading.
GLP-1s have never been approved for Medicare coverage for weight loss. The proposal to add them was new, and the Trump administration simply chose not to act on it. More importantly, the use of the phrase "long overdue" is a rhetorical device meant to imply decisive action against an established policy failure. But no such policy existed. This kind of framing is strategic. It’s designed to make followers feel like something was heroically undone, when in fact, all that happened was the rejection of a proposal that hadn’t gone into effect.
This tactic is common in wellness influencer circles, and in propaganda more broadly. It reframes inaction or regression as if it's a bold corrective measure. By using confident language to describe something that didn’t actually happen (like canceling a non-existent policy), it creates the illusion of progress or strength. This might seem benign, but it’s not. This is how narratives are crafted to shape perception. When enough of these moments accumulate, they distort the public's understanding of who is helping, who is profiting, and who is being left behind.
2. It sets up a false choice: meds or lifestyle.
One of the most persistent tactics in the wellness influencer playbook is to present pharmaceuticals and lifestyle interventions as mutually exclusive. Dr. Hyman’s framing that we should never put weight loss drugs “ahead of real, whole food, movement, and sleep,” suggests that covering GLP-1s somehow displaces or diminishes the value of lifestyle strategies. But that’s not how Medicare works, nor how health behavior change works.
Medicare already covers a variety of lifestyle-focused interventions:
Intensive behavioral therapy for obesity
The Diabetes Prevention Program (DPP), which is a structured behavior change intervention to help people eat more healthful and be more active
Medical nutrition therapy (MNT) for diabetes and kidney disease
Cardiac rehabilitation with dietary and exercise components
Preventive services that include counseling for physical activity, diet, and tobacco cessation
These are core parts of what Medicare already reimburses. Adding GLP-1 coverage doesn't mean these tools are being replaced. It means we're building a more complete toolkit.
In fact, research shows GLP-1s may enhance the effectiveness of lifestyle changes by helping patients reduce cravings, feel full longer, and make new behaviors stick. For many, these drugs make healthy eating and exercise more accessible, not less. Presenting this as an either/or proposition is inaccurate and harmful. We can support access to medication and healthy food. We can recognize the value of movement and metabolic support. The idea that we must choose one over the other is a distraction from what real, comprehensive care actually looks like.
3. If it's a "last resort," shouldn't it be accessible when people reach that point?
Dr. Hyman says GLP-1s shouldn't be a first-line treatment. But right now, many people can't access them even as a last resort. Without Medicare coverage for obesity alone, the only people who can afford these medications are those with generous private insurance or the ability to pay $1,000 to $1,200 per month out of pocket. That means a powerful tool is only available to the most privileged patients.
To be fair, Medicare does cover GLP-1s for people with type 2 diabetes or certain other conditions. But that doesn’t help the millions of Americans who are living with obesity and at high risk of developing chronic disease—yet don’t meet the specific diagnostic criteria. A person with severe obesity, joint pain, prediabetes, and hypertension may still not qualify. So even as a so-called last resort, access is incredibly limited.
And yet, it's lower-income communities - and disproportionately, Black, Latino, and Indigenous populations - who are most impacted by obesity and chronic diseases like type 2 diabetes and cardiovascular disease. These are also the populations least likely to have private insurance that covers GLP-1s and least able to afford them out of pocket. When wellness influencers argue that GLP-1s should be reserved as a "last resort," they ignore that for millions of Americans, that last resort doesn’t exist.
Instead of addressing this, many wellness narratives ignore the structural barriers that make access to care uneven. It’s not about choosing between drugs and food. It’s about whether we’re willing to make proven tools available to the people who need them most. If we want to be serious about health equity, we have to be serious about access, especially for the people most affected.
4. "Root cause" rhetoric ignores the science.
GLP-1s target the hormonal, neurological, and metabolic underpinnings of obesity: the root causes. They're not just appetite suppressants. These medications influence key pathways that regulate insulin secretion, blood glucose levels, gastric emptying, appetite control, and inflammation. In doing so, they directly address the dysregulation that contributes to obesity and many of its related chronic conditions.
Clinical trials and meta-analyses have shown that GLP-1s significantly improve glycemic control, reduce blood pressure and cholesterol, and lower the risk of cardiovascular events. Newer formulations even show promise in preserving kidney function and reducing systemic inflammation. Calling these drugs “symptom-treaters” ignores the actual research and recent breakthroughs that demonstrate their role in correcting the very mechanisms that drive chronic metabolic disease. If our goal is to address root causes, the science suggests GLP-1s belong in that conversation, alongside food, movement, sleep, and stress support, not outside it.
5. The Wellness World's Double Standard
Dr. Hyman says we should never put weight loss drugs ahead of "real, whole food, movement, and sleep." But that’s exactly what his supplement empire does every single day. On his website, he sells hundreds of products, including dozens under the category "Weight and Metabolism.”
For example, the $75 monthly supplement CraveArrest markets itself as "anti-craving support,” promising appetite control. The $73 monthly supplement EndoTrim is positioned as the solution for anyone “wishing to improve body composition.” The website also has dozens of other supplements, like Fatty15, which is promoted for "healthy glucose handling" and "healthy cholesterol levels." These are claims squarely in the realm of metabolic health, yet they’re made for supplements that are far less scrutinized and regulated than FDA-approved medications.
So when Dr. Hyman criticizes GLP-1s for being placed “ahead of” lifestyle change, the question isn’t whether we should lead with food or movement, it’s why he thinks his unregulated, unproven, high-margin supplements are exempt from that same critique. He’s not against profit. He’s not even against biochemical intervention. He’s just against FDA-approved pharmaceutical interventions that he doesn’t personally benefit from.
That’s not a principled stand. That’s a business model. And it exposes that this is not a debate about root causes or public health, but a turf war between two industries that profit from promising better health. One is heavily regulated and evidence-based. The other is free to say almost anything and charge whatever it wants.
So let’s be clear: the message isn’t “don’t turn to Pharma.” It’s “turn to me instead. And bring your credit card.”"
Beyond the Binary: A Smarter Path Forward
As someone with a PhD in nutrition science whose research focused on using diet and lifestyle interventions to reduce risk of type 2 diabetes and cardiometabolic disease, I obviously fully support doing everything we can to decrease barriers and improve adoption of behavior change to support metabolic health. And that includes expanding access to evidence-based tools, whether that’s nutrition counseling, peer support programs, or medication.
More and more research suggests that GLP-1s are not only helping improve markers like HbA1c, blood pressure, and cardiovascular risk, but are also uniquely effective at helping people finally implement the lifestyle changes that are often recommended but rarely maintained. Appetite regulation, reduced food noise, and increased satiety are biologically meaningful shifts that help people overcome some of the biggest barriers to behavior change.
One recent modeling paper even proposed a promising hybrid approach to use full-dose GLP-1s during the active weight-loss phase, followed by a structured maintenance phase that includes behavioral support, nutrition guidance, and, if needed, lower-cost or lower-dose medications. This kind of phased strategy could help reduce costs while expanding access, without cutting people off from tools that are working.
We don’t have to fall for false dichotomies pushed by MD wellness influencers who have a vested interest in steering people away from regulated medications and toward their own unregulated supplements. We can demand better. We can advocate for both access and accountability.
So instead of letting the debate stall in binaries, we can push for:
Broader access to both medications and nutrition counseling
More investment in behavior support infrastructure, before, during, and after medication use
Honest conversations about who profits from health messaging. And who gets left behind when we choose ideology over access
Final Thought
It’s easy to criticize “Big Pharma.” It’s harder to hold “Big Wellness” to the same standard, especially when the loudest voices are profiting from the alternatives they promote.
When a regulated, evidence-based tool like a GLP-1 is framed as dangerous or lazy, while $75 “anti-craving” supplements are marketed without oversight, we’re not having an honest conversation about health. We’re witnessing a strategic distraction meant to make us distrust medical advancements and turn instead to the wellness industry, which positions itself as the benevolent, altrusitic alternative while quietly profiting from unregulated products with sweeping claims.
And it’s not just a few products. According to the New York Times, Dr. Hyman made over $28 million in 2023 alone from supplement sales, lab testing, and other wellness offerings. This isn’t about principled health advocacy. It’s about protecting a very lucrative business model.
The truth is that we need all the tools. Food, movement, medication, counseling.
Support. Access. Equity.
What we don’t need is a wellness industry that thrives on false choices and builds its brand by opposing science-backed care, especially when that care might threaten its bottom line.
The next time someone claims to have the real fix, look a little closer. Because what’s marketed as a moral crusade against pharma is often just another sales pitch in disguise.





As a pharmacist for over 10 years, I appreciate this post and all of your posts. You’re one of the only reasons I’m not losing my mind when I look at social media these days. Thank you for being so outspoken with everything I’ve been trying to say and doing it so eloquently. You are my hero right now.
Thank you for this article! I’m learning more and more about these issues and appreciate the thoughtful discussion you provide. I’m grateful I’ve found your work in the midst of the MAHA noise.