Today, in his inaugural address, President Trump made a bold promise: to ‘end the chronic disease epidemic.’ This declaration reflects a key focus of the Make America Healthy Again movement, spearheaded by RFK Jr., which struck a chord with voters across the political spectrum eager for solutions to our nation’s declining health.
And the concern is understandable. Today, more than half of American adults live with at least one chronic condition—such as heart disease, diabetes, or cancer—and nearly 30% manage multiple chronic illnesses. These diseases aren’t just the leading causes of death and disability in the U.S., accounting for 7 out of 10 deaths annually; they also strain our healthcare system and economy, costing billions in treatment and lost productivity.
Certainly, the fact that we are living longer with significantly fewer deaths from infectious diseases and acute illness result in increases in age-related chronic conditions. However, many chronic conditions are preventable—or at least delayable—through lifestyle changes and early intervention. Tackling these conditions could significantly improve quality of life, healthspan, and economic productivity, while saving the healthcare system enormous resources.
If the Trump administration aims to fulfill its promise, it’s worth exploring the root causes of chronic disease in the U.S. - many of which are deeply embedded in our daily lives, our food systems, and our healthcare infrastructure - and the evidence-based solutions that could reverse this growing epidemic.
The Problem: Why Chronic Disease is So Prevalent
The chronic disease epidemic in the United States is the result of decades of policies and systems that prioritize profits over public health. It isn’t just a medical issue - it's a societal and economic crisis that affects every aspect of our lives.
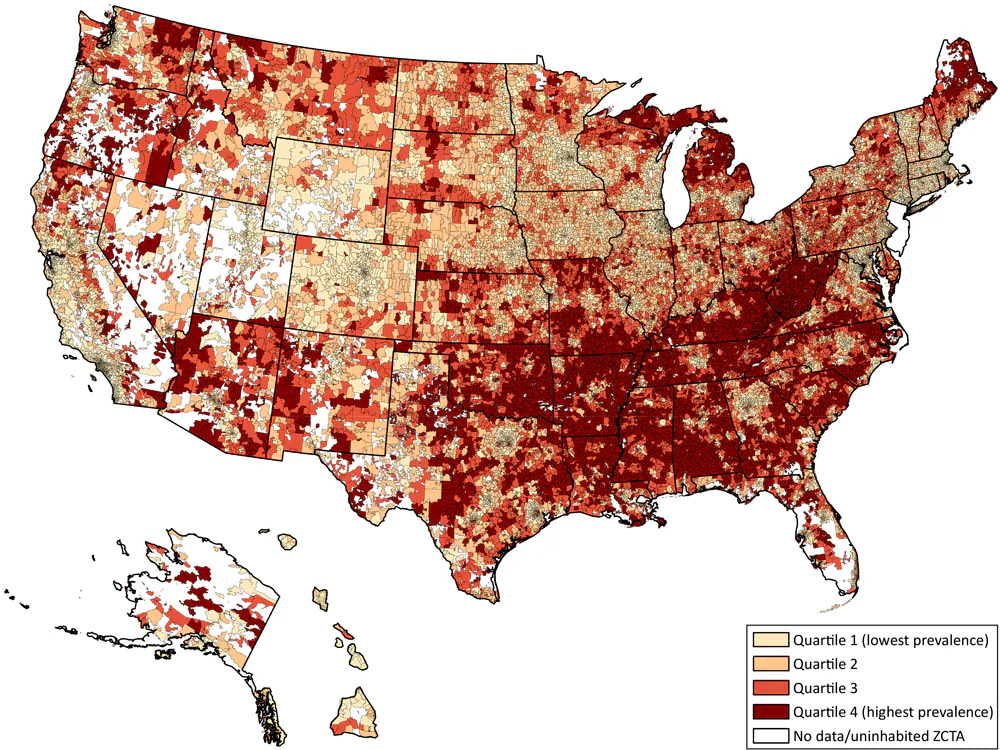
And low-income populations are disproportionately affected by the chronic disease epidemic, facing higher rates of obesity, diabetes, heart disease, and other preventable conditions. This disparity has led to a staggering 15-year life expectancy gap for men and 10-year gap for women between the highest and lowest income groups in the United States.
Many chronic conditions are driven by lifestyle factors that are directly influenced by systemic issues. And addressing chronic disease isn’t just about individual choice - it requires systemic change.
Diet and Nutrition
Individual Level: Eating a diet rich in vegetables, fruits, legumes, whole grains, protein and fiber, while reducing consumption of low nutrient, ultraprocessed foods and added sugars.
Systemic factors:
Agricultural subsidies: U.S. agricultural subsidies favor commodity crops (corn, soy, wheat) used in ultraprocessed foods, making them cheaper and more accessible than fresh produce, while less than 1% of subsidies go towards fruits and vegetables.
Food deserts: Low-income neighborhoods often lack access to fresh, affordable produce (food deserts).
Economic instability: Financial hardship forces many families to prioritize calorie-dense, ultraprocessed foods over nutrient-rich options due to cost and affordability. Limited budgets and trade-offs between food and other necessities exacerbate poor dietary choices.
Marketing & Advertising: Aggressive marketing of ultraprocessed foods, particularly to children, which influences dietary habits.
School Food Policies: School meal programs often rely on ultraprocessed foods due to cost constraints. For example, the national reimbursement rate for the national school lunch program is only $4.01 per meal (in the contiguous 48 states).
Physical Activity
Individual level: Engage in regular physical activity, including cardiovascular and strength training, and reduce sedentary behavior.
Systemic factors:
Urban design and infrastructure: Lack of walkable neighborhoods, bike paths, and safe public spaces discourages physical activity.
Transportation policies: Reliance on cars over public transit limits opportunities for incidental exercise like walking.
Workplace culture: Sedentary jobs and long working hours leave little time or energy for physical activity.
School systems: Declines in physical education programs and recess reduce activity levels in children.
Economic stability: Limited financial resources may prevent access to gyms, sports programs, or even adequate footwear and clothing for exercise.
Stress and Mental Health
Individual level: Manage stress through techniques like mindfulness, therapy, exercise, and social support. And recognize and address mental health conditions, like depression and anxiety.
Systemic factors:
Economic instability: Financial stress due to low wages, job insecurity, and medical debt exacerbates chronic stress.
Housing and neighborhood safety: Living in unsafe or overcrowded conditions increases stress and mental health risks.
Access to mental health services: Limited access to affordable mental health care leaves many conditions untreated.
Sleep
Individual level: Prioritize 8-9 hours of sleep per night and maintain good sleep hygiene, such as limiting screen time before bed and managing stress.
Systemic factors:
Work and school schedules: Early start times for schools and long or irregular work hours disrupt sleep patterns.
Economic inequities: Working multiple jobs or shift work, often held by low-income workers, can lead to sleep deprivation and irregular sleep schedules.
Housing conditions: Overcrowding, noise, or unsafe living environments can interfere with quality sleep.
Preventive Healthcare
Individual level: Attend regular checkups and screenings to ensure health conditions are caught to enable early intervention for health conditions.
Systemic factors:
Healthcare access: Lack of insurance or high out-of-pocket costs prevent many from accessing routine care
Healthcare deserts: Rural and underserved urban areas often lack healthcare providers or facilities
Cultural and language barriers: Some populations face challenges navigating the healthcare system due to language or cultural differences.
Substance Use
Individual level: Avoid or reduce use of harmful substances like tobacco, excessive alcohol, and recreational drugs.
Systemic factors:
Tobacco and alcohol marketing: Aggressive advertising, especially in low-income communities, promotes consumption.
Taxation and regulation: Policies like tobacco taxes and limits on alcohol sales can influence consumption.
Mental health and addiction services: Limited access to affordable addiction treatment perpetuates substance abuse.
The Solution: Evidence-Based Policy Changes
If the Trump administration is serious about fulfilling its promise to “end the chronic disease epidemic,” it will need to go beyond encouraging individual behavior changes and ingredient swaps in ultraprocessed food. Chronic diseases don’t occur in isolation—they arise from a food, healthcare, and economic system that prioritizes corporate profits and growth over public health.
Addressing the root causes of chronic disease requires bold policy interventions that focus on systemic change. These policies must aim to reshape our food environment, promote physical activity, expand access to healthcare, and tackle the broader social determinants of health that disproportionately harm low-income populations.
Some of those evidence-based policy changes include:
Diet and Nutrition (The Food Environment)
Reforming agricultural subsidies towards fruits, vegetables and legumes to make nutrient-rich foods more affordable and accessible
Strengthening local food systems and enhancing food access in underserved communities
Investing in and supporting modern agriculture and food science advancements that can make nutritious food more affordable
Addressing food deserts through infrastructure and incentives to encourage grocery stores to open in underserved areas
Addressing income inequality and expanding support programs like SNAP
Restricting and regulating ultraprocessed food marketing to children and mandating clear and easy to understand food labels
Increasing the reimbursement rate for school lunches an investing in farm-to-school programs
Investing in nutrition education and public health campaigns
Limiting corporate lobbying, so that they no longer have such an incredible amount of influence over our food environment and public health
Physical Activity (The Built Environment)
Invest in urban infrastructure, such as sidewalks, bike lanes, parks, and public transit, to encourage incidental exercise
Incentivize active transportation through tax credits/subsidies for biking and public transit use, and support “Safe Routes to School” programs
Revitalize physical education in schools and fund recess programs
Stress and Mental Health
Address income inequality through policies like expanding the minimum wage and expanding tax credits for low and middle income households
Expand access to mental health services by increasing funding for community mental health centers and requiring mental health coverage parity in insurance plans
Invest in affordable housing programs and initiatives to reduce overcrowding and improve neighborhood safety
Sleep
Reform work and school schedules by advocating for later school start times to align with adolescent sleep patterns, and encourage workplace policies that limit excessive overtime hours and potentially change the 40 hour work week
Limit shift work and ensure adequate rest periods between shifts for industries employing low-wage workers
Improve housing environments, and reduce overcrowding and noise in low-income housing by increasing funding for affordable housing programs
Preventive healthcare
Expand healthcare access to cover all Americans
Address healthcare deserts by offering things like loan forgiveness for healthcare providers that work in underserved areas and funding mobile clinics
Substance Use
Strengthen regulation and increase taxation on tobacco and alcohol to discourage consumption
Expand addiction treatment for recovery programs
Ban advertisements for alcohol and tobacco products
These are just some of the major policies that could begin to address the systemic changes needed to improve public health in the United States and truly reduce rates of chronic disease.
If the Trump administration is to truly “end the chronic disease epidemic,” it must recognize that individual behavior change alone won’t solve the problem. Chronic disease is rooted in systemic issues, and the solutions must be systemic as well. Bold actions to reform agricultural subsidies, redesign our cities, expand healthcare access, and tackle economic inequality could create meaningful, measurable progress—especially for those communities who have been left behind for far too long.
The Make America Healthy Again movement has captured public attention, but progress requires more than soundbites or superficial fixes. These evidence-based policies offer a clear path forward to address the root causes of chronic disease and improve the health of all Americans.





Well written break down of the systemic issues affecting health. I’m concerned, however, that this focus is leaving out the chronic health issues that are due to things like genetics and infection associated chronic illnesses. As someone with ME/CFS, none of the things you mention would have prevented nor will cure my illness. (Though some help decrease symptoms.) Scientific research on causes & cures are also necessary. I fear an RFK lead HHS will lead to less research and more personal blame for an already greatly misunderstood illness like ME/CFS & other autoimmune & chronic illnesses like MS, Lupus, & Crohns et al.
I’m a pediatrician who works in a low-income clinic and could not agree with you more! Thank you! Thank you!!!!